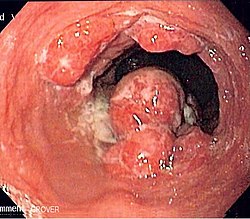
Radiation Oncology/Esophagus/Overview
Appearance
|
Front Page: Radiation Oncology | RTOG Trials | Randomized Trials |
|
|
Esophagus: Main Page | Staging | Overview | Resectable | Unresectable | Randomized | |
Esophageal Cancer Overview
Epidemiology
[edit | edit source]- Esophageal Cancer
- Incidence: 15,600 cases in US (2007 Estimate)
- Incidence rate about 200-260 per 100,000
- Higher incidence in men 4x (12.1k vs. 3.4k)
- Higher incidence in African Americans by 5x
- Deaths: 13,900 deaths in US (2007 Estimate)
- Percentage and overall incidence of adenocarcinomas is increasing; increasing number of cancers involving the distal esophagus.
- 1/3 of H&N cancer patients who develop a second primary tumor will have esophageal cancer.
- Barrett's esophagus risk for developing adenoCa is significantly higher (14-150x) over general population, and corresponds ~0.5% per year. Progression is more likely with development of dysplasia within the metaplastic area, occurring in ~20% patients
- Leeds; 2007 (UK) PMID 17890521 -- "Risk of Mortality and Cancer Incidence in Barrett's Esophagus." (Cook MB, Cancer Epidemiol Biomarkers Prev. 2007 Oct;16(10):2090-6. Epub 2007 Sep 21.)
- Retrospective. 502 patients with BE. Standardized mortality ratios (SMR) and standardized incidence rates (SIR) estimated
- Outcome: Overall mortality elevated (SMR 1.21), even after excluding esophageal CA (1.16). Risk for esophageal CA mortality (SMR 7.3), digestive tract diseases (SMR 2.0)
- Esophageal CA incidence rates: overall esophageal CA SIR 8.7, esophageal adenoCA 14.3
- Conclusion: Increased risk of esophageal CA incidence (9x; for adeno 14x) and mortality (7x)
Risk Factors
[edit | edit source]- Tobacco
- Alcohol
- Fruits and vegetables - protective
- Socioeconomic status - low is worse, particularly in African American men
- Obesity - worse for adeno
- GERD - associated with development of Barrett's
- H. pylori - protective for adeno
- Barrett's esophagus - single most important risk factor for adeno
- Tylosis - autosomal dominant, tylosis esophageal cancer (TOC) gene, develop esophageal papillomas, and at extremely high risk of developing esophageal cancer
- Plummer-Vinson - approximately 10% develop hypopharynx or esophagus cancer
- Caustic injury
- Achalasia
- Prior aerodigestive tract malignancy
Anatomy
[edit | edit source]- Length is about 25 cm. Esophageal lesion distance on EGD is typically given from incisors
- Clinically important distance is from incisors to GEJ, which is ~40 cm.
- Layers:
- Mucosa: epithelium, lamina propria, muscularis mucosa. Separated by basement membrane from rest of esophageal wall
- Submucosa: fibroelastic fibers, nervous plexuses, glands
- Muscularis propria: inner circular muscle layer, outer longitudinal muscle layer
- Adventitia: dense periesophageal connective tissue
- The serosa only lines the intra-abdominal esophagus
- AJCC divisions of the esophagus: (These are based on adjacent surgical landmarks)
- Cervical esophagus:
- Hypopharynx to the thoracic inlet, which is at the level of the sternal notch.
- By endoscopy, 15 to <20 cm from the incisors
- If thickening of the esophageal wall begins above the sternal notch, the location is cervical
- Upper thoracic esophagus:
- Thoracic inlet to lower border of the azygos vein
- By endoscopy, 20 to <25 cm
- Middle thoracic esophagus:
- Lower border of the azygos vein to the inferior pulmonary veins
- By endoscopy, 25 to <30 cm
- Lower thoracic esophagus and EG junction:
- Inferior pulmonary veins to the stomach; includes the intraabdominal portion of the esophagus
- By endoscopy, 30 to 40 cm
- For cancers arising near the EGJ, they are staged as esophageal/EGJ if the epicenter is in the lower thoracic esophagus, the EGJ, or within the proximal 5 cm of the stomach (cardia) and extend into the EGJ or esophagus
- Those with an epicenter in the stomach greater than 5 cm distal the EGJ, or those within 5 cm of the EGJ but that do not extend into the EGJ or esophagus, are staged as gastric
- Siewert classifaction is disregarded
- Cervical esophagus:
- Historical divisions of the esophagus
- Cervical esophagus - begins at cricopharyngeal muscle, 18 cm from the incisors (C7 level), to the thoracic inlet, 20-24 cm from incisors (T3 level).
- Thoracic esophagus - from thoracic inlet, 24 cm from incisors (T3), to GE junction (usually T10 or T11).
- Upper thoracic - T3 to T4, 20 cm to 25 cm - thoracic inlet to carina
- Mid thoracic - T5 to T8, 25 cm to 35 cm - carina to inferior pulmonary vein
- Lower thoracic - T9 to T10, 35 to 40 cm - below pulmonary vein
- GE junction: (Classification by Siewert: PMID 11525305, PMID 9823902), center within 5 cm proximal/distal to GEJ
- Type I (distal esophagus) - arises from area with specialized intestinal metaplasia of the esophagus. Commonly, center of the tumor located 1 - 5 cm above the gastroesophageal junction
- Type II (cardia, considered gastric) - arises from the cardiac epithelium or short segments with intestinal metaplasia at the GEJ. Commonly, center of the tumor located 1 cm above to 2 cm distal to GEJ
- Type III (sub-cardia, considered gastric) - arises from subcardial location and infiltrates GEJ from below. Commonly, center of tumor >2 cm distal to GEJ
- Resectability often limited:
- Lack of fibrous serosa to prevent local spread
- Rich lymphatic network in submucosa and muscularis that allows longitudinal and circumferential drainage
- Frequent medical comorbidities
Barrett's Esophagus
[edit | edit source]- Multi-Institutional -- RFA vs. Sham procedure
- Randomized, 2:1. 127 patients, dysplastic Barrett's esophagus. Arm 1) RFA vs. Arm 2) Sham procedure. Primary outcome 1-year rate of dysplasia/metaplasia
- 2009 PMID 19474425 -- "Radiofrequency ablation in Barrett's esophagus with dysplasia." (Shaheen NJ, N Engl J Med. 2009 May 28;360(22):2277-88.)
- Outcome: In low grade dysplasia patients: complete eradication RFA 90% vs. sham 23% (SS). In high grade dysplasia patients 81% vs. 19% (SS). Disease progression RFA 4% vs. sham 16% (SS), cancer development 1% vs. 9% (SS)
- Toxicity: More chest pain, 1 patient UGI bleeding, 6% esophageal stricture
- Conclusion: RFA associated with a high rate of complete eradication of dysplasia and intestinal metaplasia, and reduced risk of disease progression
Presentation
[edit | edit source]- 50% present with local or locoregional disease.
- Fewer than 60% of pts with locoregional disease are operable.
Patterns of spread
[edit | edit source]LN involvement risk is 20% for cervical tumors, 50% for mid thoracic, 30% for distal.
Extensive longitudinal interconnecting system of lymphatics.
- LN+ risk by location:
- Cervical esophagus - 69% peritracheal & periesophageal. Only 6% supraclav, 9% abdominal LN.
- Upper thoracic - 29% superior mediastinal nodes, 27% middle mediastinal nodes, 29% lower mediastinal nodes, 32% abdominal nodes
- Middle thoracic - 11% superior mediastinal, 21% middle mediastinal, 18% lower mediastinal, 40% abdominal nodes
- Lower thoracic - 10% superior mediastinal, 14% middle mediastinal, 27% lower mediastinal, 70% abdominal nodes
- LN+ risk by stage
- T1a - 7%
- T1b - 20%
- T2 - 40%
- Overall distant metastasis rate 50%. Most commonly to the lung and liver.
- Southern Tohoku, Japan; 2009 (1989-2008) PMID 19042946 -- "Determination of the irradiation field for clinical T1-T3N0M0 thoracic/abdominal esophageal cancer based on the postoperative pathological results." (Nakamura T, Jpn J Clin Oncol. 2009 Feb;39(2):86-91. Epub 2008 Nov 28.)
- Retrospective. 95 patients, clinical T1-T3N0 thoracic/abdominal esophageal cancer. Squamous cell 85%, adeno 9%. Rate of pathologic LN involvement evaluated
- Outcome: Positive LN 42% (upper 37%, middle 32%, lower 46%, abdominal 70%).
- Radiation fields: Extent of irradiation fields for each subsite determined
- Conclusion: Lymph node mets seen often in cT1-T3; optimal fields designed
Prognosis
[edit | edit source]- No treatment: 6 month OS 20%, 5-year OS 0%
- Surgery alone: 5-year OS 20-25%
- Stage I: 5-year OS 80-90%
- Stage IIA (T2-T3 N0): 50%
- Stage IIB (T1-T2 N1): 20%
- Stage III (T3-T4 N1): 10-15%
- Stage IVa (M1a): 10%
- Palliation of dysphagia with surgery - 80%.